Melissa M. Gonzalez, Psy.D.
Often times, parents are shocked to learn that their child has an eating disorder. Eating Disorders (EDs) aren't always easy to identify as so many practices of disordered eating are secretive. Some parents believe that their children are simply engaging in typical dieting rituals, some have never observed an episode of binge eating or purging, some might think their child is too young for body concerns, and some simply can't believe that their child is capable of harming themselves in such a serious way. Nonetheless, early intervention is crucial and parents must learn to be savvy to ensure that their children get the necessary treatment. There are many warning signs that parents can look for in deciding if they need to seek help.
Poor self-esteem, a distorted body image, or unrealistic views of their physical appearances are almost always present. When children eat behind closed doors or in secret or when food is missing there may be cause for concern. Hoarding of foods, perhaps in preparation for a binge, also occurs in some cases. Some children may exihibit signs of guilt or shame after eating. They may avoid eating in public or in front of other people. For those who are purging, they typically excuse themselves quickly from the table and visit the restroom soon after eating. They may run the water in the shower or in the sink in order to cover up the sound of vomiting. Also, tooth decay is often a problem. Glands in the neck may be swollen and cheeks may appear puffy. Broken blood vessels may be observed in the eyes and they may also complain of a sore throat. Hair loss, paleness, and dizziness may also occur due to malnutrition. Less obvious methods of purging include use of laxatives and excessive exercise. When significant weight loss occurs, children may frequently complain of being cold. They may hide their shrinking bodies beneath layers of oversized clothing. Females may stop menstruating normally. Additionally, individuals with EDs may have an intense need for control or strong perfectionistic tendencies. Extreme or dramatic mood swings are also common and may be a sign of co-occuring mental disorders.
If you suspect that your chld may suffer from an eating disorder or may be developing patterns of disordered eating, express your concerns difectly and privately in a kind, empathic, calm and supportive manner. Be able to ask educated questions. Do not try to force your child to eat. Engaging in a power struggle will not help. Providing advice about dieting or nutrition commenting positively about appearance, or attempting to solve your child's problems is not recommended. Do not agree to keep disordered eating habits a secret. Finally, do not let fear prevent you from confronting your child. EDs have the highest mortality rate of any psychiatric illness. Intervening and seeking help may save your child's life. We here at the Tarnow Center for Self-Management believe in a comprehensive approach to the treatment of eating disorders. This "attack n all fronts" often includes family therapy; and parents become an important part of the treatment process. Additionally, parents are encouraged to seek support, for themselves during this challenging process and that may take the form of support groups including other parents of children with EDs, use of online resources, or even individual therapy.
Melissa M. Gonzalez, Psy.D.
A 2008 meta-analysis of 77 studies found that exposure to media images depicting a thin ideal-body is related to body image concerns for women including body dissatisfaction, internalization of the thin ideal, and certain eating behaviors or beliefs. Most of the images we are exposed to by the media – including television, movies, magazines, websites, and advertisements – depict women who are very different from the average American woman.
Media portrayals of thin perfection permeate our society, but don’t reflect who we truly are. While the average American woman is 5’4” and weighs 140 pounds, the average American model is 5’11” and weighs only 117 pounds. This puts her at around 75% of her ideal body weight. Diagnostic criteria for anorexia nervosa requires a body weight that is less than 85% of the ideal body weight, meaning that most models would easily meet such criteria. Furthermore, these models wear makeup and clothing that enhances and/or diminishes certain parts of their bodies. Many have had plastic surgery or other procedures to alter their appearance. Still, editing and enhancing techniques, such as Photoshop, are used to further distort these images into unrealistic representations of beauty. Bodies that differ from this standard with regard to age, color, or shape are not equally represented. These images are ever-present in our lives and they shape the way young women and girls believe their bodies should look. What’s worse is that young women and children are often targeted by these media messages.
We have to challenge these ideals and help girls develop as sense of self that is rooted in more than just physical appearance. We cannot accept these representations as expectations, instead teaching acceptance and love of bodies that come in all shapes and sizes. We can promote health and fitness in a manner that does not contribute to disordered eating. We must learn to value ourselves and our bodies for more than just beauty by someone else’s definition.
The role of the media in body image concerns among women: A meta-analysis of experimental and correlational studies. Grabe, Shelly; Ward, L. Monique; Hyde, Janet Shibley Psychological Bulletin, Vol 134(3), May 2008, 460-476.
If you suspect that your chld may suffer from an eating disorder or may be developing patterns of disordered eating, express your concerns difectly and privately in a kind, empathic, calm and supportive manner. Be able to ask educated questions. Do not try to force your child to eat. Engaging in a power struggle will not help. Providing advice about dieting or nutrition commenting positively about appearance, or attempting to solve your child's problems is not recommended. Do not agree to keep disordered eating habits a secret. Finally, do not let fear prevent you from confronting your child. EDs have the highest mortality rate of any psychiatric illness. Intervening and seeking help may save your child's life. At the Tarnow Center for Self-Management we believe in a comprehensive approach to the treatment of eating disorders. This "attack n all fronts" often includes family therapy; and parents become an important part of the treatment process. Additionally, parents are encouraged to seek support, for themselves during this challenging process and that may take the form of support groups including other parents of children with EDs, use of online resources, or even individual therapy.
Melissa M. Gonzalez, Psy.D.
We all know what starvation looks like on the outside, whether we envision some child in a poverty-stricken, third-world country or a teenage girl with Anorexia Nervosa (AN). When most of us think about severe AN, we have visions of painfully thin girls and women with protruding bones, thinning hair, sunken eyes, and hollow cheeks. We can look at her and see what AN looks like, but what we don’t see is the damage being done on the inside. Today, I want to talk specifically about the impact of starvation on the brain and brain functioning. A starving brain operates very differently from a normal, well-fed brain; and changes in physiology and metabolism often result in distorted thinking. Such consequences may exacerbate the existing symptoms of eating disorders, create new challenges, or make treatment even more difficult. Therefore, it is important to understand this process and the changes that occur.
When the body begins to experience starvation, as is the case in AN, the body makes every effort to preserve the brain and provide it with the nutrients it requires to continue functioning. The idea here is to keep the brain going so it can direct the body to go seek out food and nutrients. So, in the initial stages of starvation, our bodies convert glycogen in the liver into more user-friendly glucose. However, after a short time, our bodies begin burning fat reserves. When our fat is metabolized into nutrients useable by the brain, Ketone bodies are produced resulting in a state of Ketosis. Eventually, after a more extended period of starvation, the body begins to run out of excess fat and must, instead, turn to muscle and connective tissue. Finally, when all else fails, the brain begins to break down neurons, reducing the volume of the brain and thereby “shrinking” the brain. While some studies suggest that brain volume can be restored after starvation ceases, other studies are beginning to find that recovery may not be so simple. It is also interesting to note that male brains seem to begin breaking down neurons more quickly in the starvation process than female brains.
What happens next? Malnutrition or starvation often results in difficulties with attention and concentration. The limbic system, which controls many aspects of our emotional response, attachment, and memory, is also impacted. Additionally, when the frontal lobes are involved, deficits in judgment, insight, and impulse control are often noticed. Brain imaging studies have noted an imbalance between the circuits that regulate our reward systems, emotions, the ability to plan ahead, and our understanding of consequences. The pleasure response often associated with food and eating may be blunted so that those who suffer with AN do not feel pleasure when eating. Instead, they may begin to experience fear, stress, or anxiety in response to food rather than feeling anxious or fearful when food is scarce or unavailable. The anorexic brain may no longer be able to signal the individual to eat in response to hunger – the message just doesn’t get through. Changes in the metabolism of neurotransmitters such as serotonin and dopamine are likely instrumental in the changes described above. So now, when we begin to treat the individual with AN, we must not only overcome the mind, but also the brain and the changes that have occurred as the result of malnutrition and food restriction. Finally, it is also important to note that in measuring the electrical activity of the brain using EEG, we find that those with AN and other eating disorders have a higher prevalence of EEG dysrhythmia. Even in those individuals without an eating disorder, EEG results showed anxiety and slow thinking in those who did not eat. When foods high in sugar or carbohydrates were consumed, slow processing speed and an inattentive pattern emerged. However, when individuals consumed a balanced, nutritious meal prior to being tested, a more normalized EEG pattern with less anxiety, impulsivity, and distractibility was observed.
So what does it all mean? First, early intervention is especially important in order to interrupt the loss of brain volume experienced by many anorexics; and the treatment of chronic eating disorders becomes more complex due to physiological and metabolic changes in the brain. Second, in assessing individuals with eating disorders, especially AN, an EEG may be useful in addition to a comprehensive psychological evaluation in order to determine the impact on the brain. Then, perhaps neurotherapy could be utilized as part of a treatment strategy if indicated. Third, in psychotherapy, distorted thinking must be understood within the context of a starving brain as well as the mental illness itself. Finally, psychiatric intervention is often an essential element of treatment in order to better regulate the neurotransmitters in the brain. Here at the Tarnow Center for Self-Management, we provide all of the services necessary to assess and treat the impact of eating disorders on the mind and the brain including psychological assessment; QEEG studies; individual, group, and family therapies; and psychiatric services. Please call us if you or someone you know is suffering with disordered eating.
If you suspect that your chld may suffer from an eating disorder or may be developing patterns of disordered eating, express your concerns difectly and privately in a kind, empathic, calm and supportive manner. Be able to ask educated questions. Do not try to force your child to eat. Engaging in a power struggle will not help. Providing advice about dieting or nutrition commenting positively about appearance, or attempting to solve your child's problems is not recommended. Do not agree to keep disordered eating habits a secret. Finally, do not let fear prevent you from confronting your child. EDs have the highest mortality rate of any psychiatric illness. Intervening and seeking help may save your child's life. We here at the Tarnow Center for Self-Management believe in a comprehensive approach to the treatment of eating disorders. This "attack n all fronts" often includes family therapy; and parents become an important part of the treatment process. Additionally, parents are encouraged to seek support, for themselves during this challenging process and that may take the form of support groups including other parents of children with EDs, use of online resources, or even individual therapy.
Melissa M. Gonzalez, Psy.D.
Dialectical Behavior Therapy (DBT) is a specialized and empirically-validated form of cognitive behavioral therapy that was developed by Marsha Linehan for the treatment of women with Borderline Personality Disorder (BPD). In it’s original form, DBT involved an intensive outpatient treatment including weekly individual therapy, weekly group skills training, weekly therapist consultation team meetings, and 24-hour access to telephone coaching as needed.
The theory underlying this treatment poses that emotionally vulnerable women, when exposed to an environment they perceive as invalidating, will experience chronic emotional dysregulation or difficulty modulating their emotional reactions. So what is meant by emotionally vulnerable? Essentially, this means an individual who has a heightened sensitivity to emotional stimuli, intense emotional responses, and difficulty returning to an emotional baseline. Consequently, when these women become emotionally dysregulated, they may have difficulty inhibiting mood-dependent behaviors (such as self-injury), organizing themselves to achieve goals independent of mood, regulating physiological arousal, diverting attention away from emotionally volatile stimuli, or simply experiencing any emotion without either avoidance or extreme secondary emotional interference. Since it’s inception, DBT strategies have been applied to the treatment of many mental disorders with similar characteristics. Since eating disorders (EDs) are often characterized by problem behaviors (e.g. restricting, bingeing, purging) that are associated with emotional dysregulation, DBT has been proposed as a treatment option for Anorexia Nervosa (AN), Bulimia Nervosa (BN), and Binge Eating Disorder (BED).
A recent journal article published in Eating Disorders: The Journal of Treatment and Prevention (April 2012) described a systematic literature review of studies citing the use of DBT or DBT-based approaches in the treatment of EDs. The findings of this review indicated that the use of treatments based on the DBT model – often modified for the specific treatment of EDs – generally resulted in positive impact on the reduction of ED behaviors, improvement in markers of mood and affect, and greater retention of individuals in treatment. These are important and promising findings as this means that clients are safer, less emotionally volatile, and more likely to continue working toward recovery. Eating Disorders are notoriously difficult to treat as clients are often highly resistant to change and treatment is often initiated by others when the individual is already in serious danger. Furthermore, since mood disorders, substance abuse, self-harming behaviors, and BPD often co-occur with EDs, DBT treatment targets are often well suited to these clients.
At the Tarnow Center for Self-Management, this type of specialized treatment can be incorporated in several ways into a comprehensive treatment approach which can include psychiatry, individual therapy, family therapy, and group therapy provided by an experienced team of clinicians. Ongoing DBT groups provide specific skills for teenage girls and their parents for the development of emotional regulation; and DBT skills can be incorporated into other areas of treatment as well. Please call us if you or someone you know is struggling with disordered eating.
If you suspect that your chld may suffer from an eating disorder or may be developing patterns of disordered eating, express your concerns difectly and privately in a kind, empathic, calm and supportive manner. Be able to ask educated questions. Do not try to force your child to eat. Engaging in a power struggle will not help. Providing advice about dieting or nutrition commenting positively about appearance, or attempting to solve your child's problems is not recommended. Do not agree to keep disordered eating habits a secret. Finally, do not let fear prevent you from confronting your child. EDs have the highest mortality rate of any psychiatric illness. Intervening and seeking help may save your child's life. We here at the Tarnow Center for Self-Management believe in a comprehensive approach to the treatment of eating disorders. This "attack n all fronts" often includes family therapy; and parents become an important part of the treatment process. Additionally, parents are encouraged to seek support, for themselves during this challenging process and that may take the form of support groups including other parents of children with EDs, use of online resources, or even individual therapy.
Melissa M. Gonzalez, Psy.D.
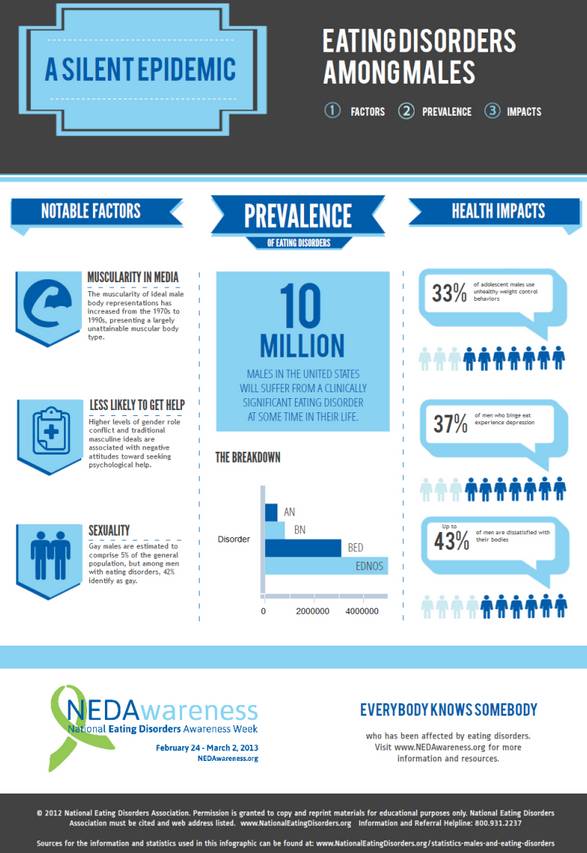
Eating Disorders (EDs) are not exclusively diagnosed in girls and women. In fact, the diagnosis of EDs in men seems to be rising. However, it is difficult to know the true prevalence of male EDs due to the stigma in our society and views of EDs as a “feminine” problem.
Consequently, many men do not get properly diagnosed or do not seek treatment at all. But some studies have indicated that as many as 1 in 4 new eating disorder cases are male. In 2002, the NIMH found lifetime prevalence rates in men of 0.3% for anorexia nervosa, 0.5% for bulimia nervosa, and 2% for binge eating disorder.
Men with EDs may share many of the same characteristics as women with EDs including low self-esteem, perfectionism, over-achieving qualities, conflict avoidance, anxiety, depression, a need for control, difficulty expressing emotions, feelings of unworthiness, feelings of self-loathing, need for acceptance, and poor body image. However, there are some important differences between men and women with EDs. First, men seem to develop eating disorders at a later age than women. Typically, men are overweight or obese before they develop an eating disorder and they are often bullied or teased about their weight as children. Men are more likely to suffer from co-occuring addictions to alcohol or substances; and they often experience more sexual anxiety. Some men develop disordered eating habits through involvement in sports that have expectations about body types or weight. For example, wrestlers are often required to drop weight suddenly in order to make a certain class and football players are often encouraged to bulk up or gain weight, be it muscle or fat. Interestingly, Dr. Arnold Anderson coined the term Reverse Anorexia or Bigorexia where an individual believes that he can never be big enough so he continues in efforts to bulk up and gain muscle mass.
The graphic below can be found at: http://nedawareness.org/sites/default/files/LearnMalesED.png